Vitrectomy: A Valuable Surgical Procedure
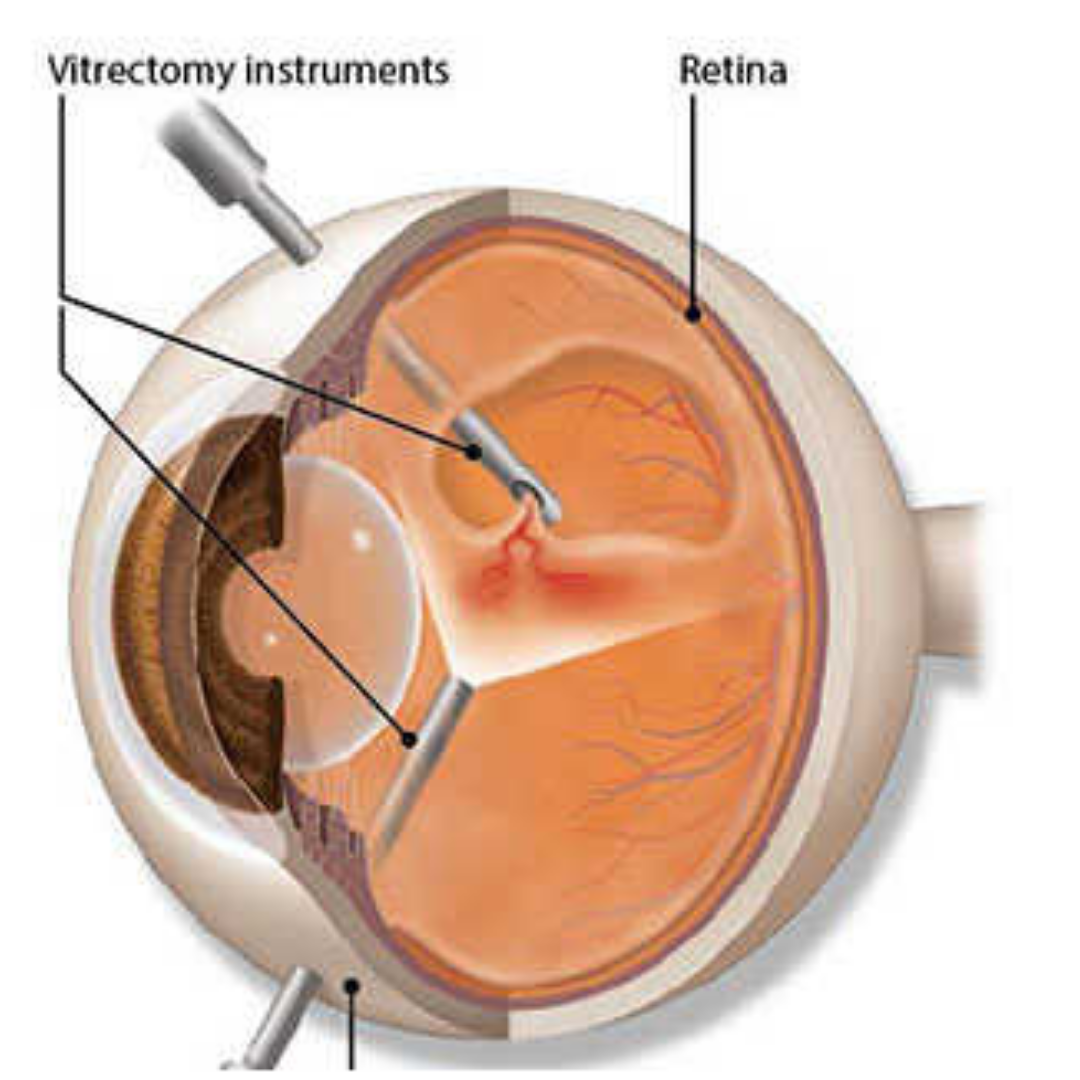
The vitreous is a transparent, colorless gel-like substance that lies in the space between the lens and the retina. Overtime, a patient may develop a specific condition that would best be managed by removing the vitreous in the eye. This surgical procedure of vitreous gel removal is known as a vitrectomy.
What Is a Vitrectomy?
A vitrectomy is a surgical procedure performed by a retina specialist to treat underlying conditions involving the retina and the vitreous of the eye. A retina specialist may offer a vitrectomy to better manage a number of conditions, including:
- Removing blood or substances hindering light from properly focusing on the retina
- Removing scar tissue that causes a wrinkle in the retina and impairs activities of daily vision
- Repair of a retinal detachment
- Removal of a foreign body as a result of injury
During a vitrectomy, the retina specialist will remove the majority of the vitreous and replace it with a saline solution. However, in special cases, a gas bubble or silicone oil may be placed in the eye instead. While the eye is healing, the body will begin naturally replacing the saline solution or gas bubble with its own aqueous humor (fluid).
When Is a Vitrectomy Recommended?
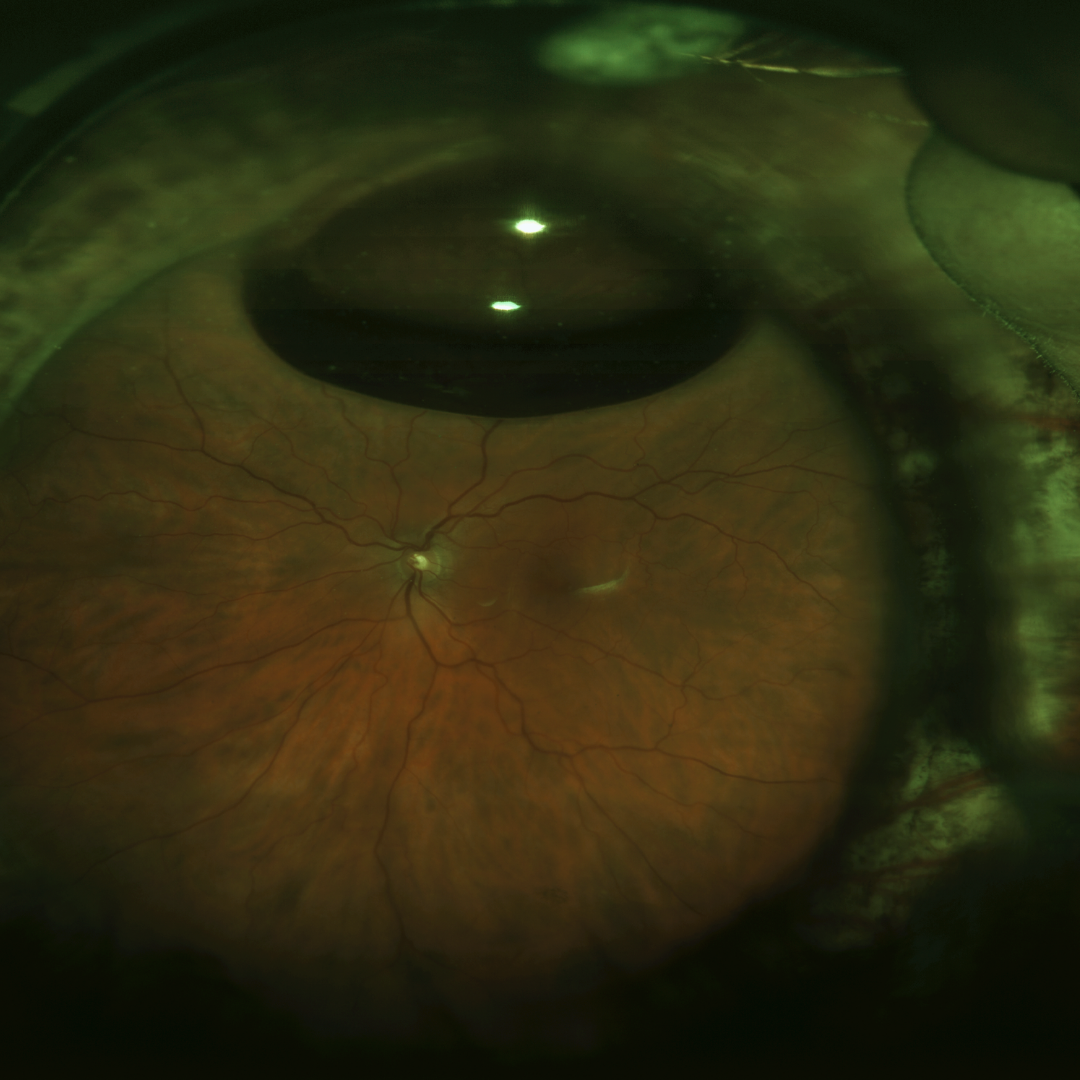
In order to determine if a patient is a good candidate for a vitrectomy, a visit to a retina specialist is necessary. During this assessment, the patient will undergo a dilated eye exam to allow the retina specialist to better assess the overall health of the eye. In-office testing is typically required to better assess a patient’s condition. Diagnostic tools such as ocular coherence tomography (OCT) and/or ultrasound will allow the retina specialist to carefully determine if a patient is a good candidate for a vitrectomy.
Many patients present with diseases or conditions that may be better managed by proceeding with a vitrectomy. Patients may be experiencing:
- Vitreous opacities (floaters) that interfere with daily activities
- Retinal detachments in which the retina has separated from the back of the eye.
- Diabetic retinopathy – a condition in which blood vessels bleed into vitreous causing dark floaters
- Macular hole
- Macular pucker – a.k.a epiretinal membrane or retinal wrinkle
- Endophthalmitis – an infection in the eye.
- Severe eye injury
- Complications that may arise during cataract surgery
In order for surgical intervention to take place for an underlying condition, four specific requirements must be met.
- The present condition threatens loss of vision
- Spontaneous healing of the specific condition is unlikely due to the severity of the condition.
- The potential benefit outweighs the possible risk of the procedure.
- The risks, benefits, and alternatives are understood and accepted by the patient.
Once the condition has been identified and these four requirements are met, you and your retina specialist can begin discussing the surgical plan.
The overall goals of a vitrectomy are:
- To treat abnormalities causing visual disturbances
- Reduce the likelihood of recurrence of an abnormality
- Minimize the risk of complications occurring from an underlying condition.
How Is a Vitrectomy Performed?
At Venice Retina, Dr. Anita Shane prides herself in utilizing advanced technology and surgical techniques during vitrectomy procedures. Due to these new advancements, vitrectomies can be completed in an outpatient surgery center. Before the procedure begins, the patient will be given IV sedation allowing them to go into a “twilight sleep”. During this time, an injection of local numbing will go around the eye to allow for maximum comfort during the procedure. A lid speculum is placed in the eye to allow the eye to remain open during the procedure. Additionally, a drape will be placed over the non-surgical eye for protection. Self-sealing, suture-less incisions are made in the white part of the eye (sclera) and three ports are inserted. The surgeon will utilize a surgical microscope with a specialized lens to allow a wide, detailed view of the inside of the eye. A device known as a vitrector is inserted into one the wounds along with the surgeon’s light source. During the vitrectomy the vitrector will help to:
- Remove cloudy vitreous
- Remove scar tissue from the retina
- Remove any foreign objects
- Return the retina to its original position against the back of the eye
Once the vitrector has cut and suctioned out all of the vitreous, a 360-degree inspection is completed to ensure there are no retinal tears or detachments. If the surgeon finds any abnormality, it can be repaired immediately preventing further complications. After the examination is complete, the ports are removed, and a patch is placed over the patient’s eye.
What Are the Expected Outcomes?
Due to small incisions and self-sealing wounds, there is little to no pain or discomfort after a vitrectomy. A patch and shield are placed over the patient’s eye to prevent injury after the procedure is complete. Your retina surgeon will recommend that the patch be worn at night to prevent possible injury while sleeping. The patient will then be required to follow-up with the retina surgeon one day after the procedure. During this visit, the patient will be placed on a drop regimen that is necessary to prevent any postoperative complications. Any additional postoperative instructions may be discussed during this visit.
Recovery after a vitrectomy has little impact on a patient’s day to day life. The saline solution that is placed in the eye after the vitreous is removed will be naturally replaced by the body’s own aqueous fluid. Also, due to smaller incisions, severe pain and/or complications are uncommon for vitrectomy procedures.
What Are the Risks?
Although severe complications are rare and uncommon, as with any surgical procedure there are risks that must be taken into account when determining if a vitrectomy is the best option for managing your condition. These risks include:
Despite these risks, there is a high anatomic success rate for vitrectomy procedures. This is owed to continuing advancements in techniques to reduce patients’ risk of postoperative complications.
- Infection
- Bleeding
- Retinal tear or detachment
- Pain
- Decrease in vision
- Cataract development in patients over the age of 50 and have not undergone cataract surgery.
What Can Venice Retina Do for You?
Dr. Anita Shane at Venice Retina is backed by years of experience in vitreoretinal surgery. With this experience, Dr. Anita Shane will ensure that you receive the best surgical care. She will help guide you through the process of determining if a vitrectomy is necessary to better manage your condition. Dr. Shane and the staff at Venice Retina are dedicated to help you every step of the way!
To hear more about vitrectomy procedures or to determine if you are a good candidate, contact us today to schedule an appointment!
