What is a Retinal Detachment?
To better understand what exactly a retinal detachment is, let us first talk about the role of the retina in our eye. For visualization purposes, think of a room with four walls. Now, think of the inside of the room being full of clear jelly and the walls lined with wallpaper. Let us compare this analogy to the eye! The inside of our eyes is filled with a jelly-like substance called the vitreous humor (like the jelly inside the bedroom), and the inside lining of our eyes is called the retina (like the wallpaper lining the walls). The retina itself is a crucial light-sensitive tissue that transmits vision to our brains through the optic nerve. A proper-functioning retina is critical to our everyday vision – without our retina, we simply would not see.
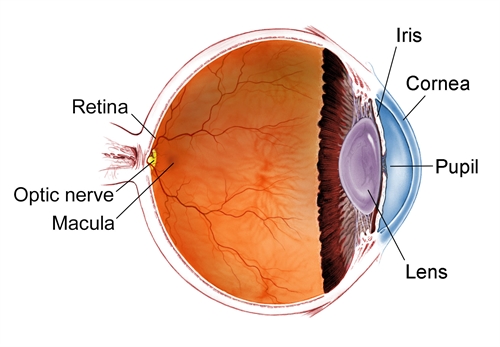
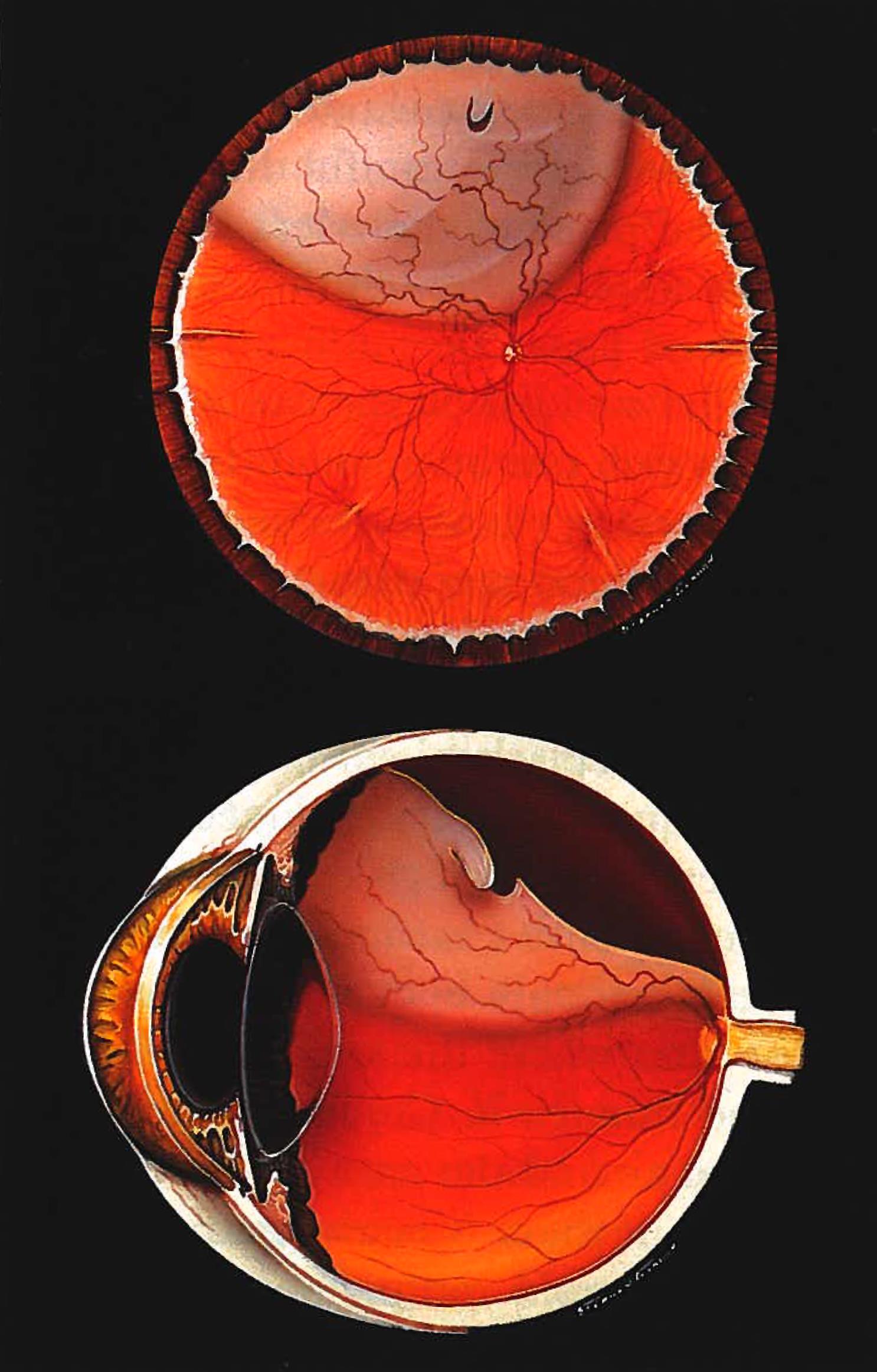
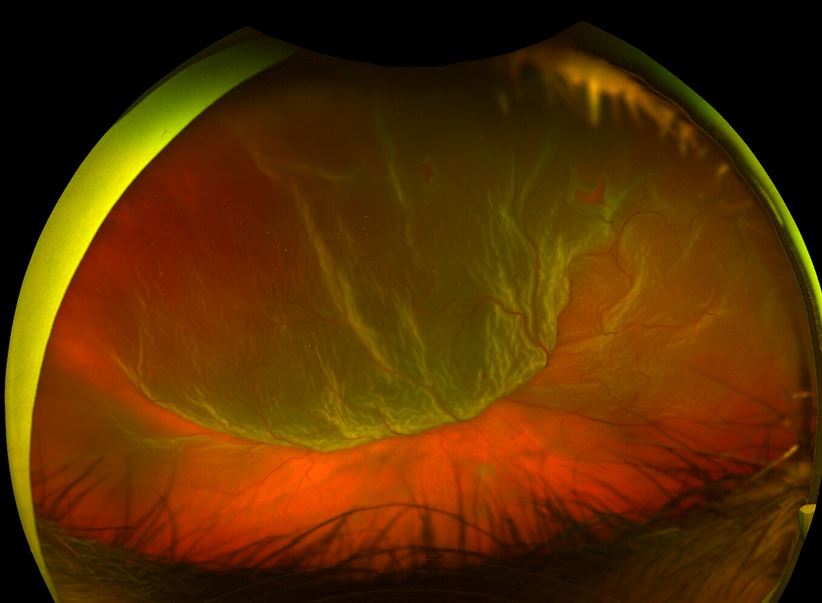
A retinal detachment is when the retina is pulled away from its normal position at the back of the eye wall and is no longer attached to its underlying nutrient layer. If you think of it regarding the previous analogy, a retinal detachment occurs when the jelly inside of the bedroom finds the space between the wallpaper and the wall, lifting the wallpaper completely off the wall itself. Retinal detachments are considered an acute threat to vision and require urgent medical attention.
Signs and Symptoms of a Retinal Detachment

If you are experiencing any of the following symptoms, it is important to seek a prompt dilated eye exam. The sooner that a retinal detachment is addressed, the better chance of a positive visual outcome.
Flashes – bursts of light inside of our eye, like a lightning bolt.
Floaters – a sudden onset of many new floaters.
Sudden, painless decrease in vision
A “curtain” in your vision. This curtain does not go away when you move your eyes around but is instead fixated in one specific part of your peripheral vision.
What Causes A Retinal Detachment?
There are a variety of risk factors that increase the likelihood of developing a Retinal Detachment.
One of the largest causes of retinal detachments is related to an event that happens in everyone’s eyes as they grow older called a Posterior Vitreous Detachment (PVD). Just as we develop wrinkles with aging, we develop a PVD as our eyes age. Naturally occurring, this is when the vitreous jelly inside of our eyes spontaneously separates from the retina. As the vitreous jelly is separating, it can pull on the retina and cause a retinal tear or detachment. This traction causes new flashes and floaters, or even a “curtain” in your vision. It is crucial to have any new flashes or floaters evaluated through a dilated eye exam as they can be signs of a retinal tear or detachment requiring urgent ophthalmologist intervention.
Some Other Risk Factors Include:
Trauma – sudden blows or perforating injuries to the eye can cause a retinal detachment.
Genetics – some people are born with a characteristically “thinner” retina, placing them at an increased risk. This can be evaluated and diagnosed through a dilated eye exam.
Prior Eye Surgery – any time you undergo eye surgery, there is an increased risk of inadvertently causing a retinal detachment.
Myopia (Near-Sightedness) – people who are near-sighted have longer-shaped eyes (similar in shape to a football) and because of this, the retina can be stretched or elongated making it more prone to retinal tears or detachments.
How Do You Diagnose A Retinal Detachment?
It is important to note that a detached retina will not be visible to the naked eye. Since the retina itself does not contain any pain fibers, if you have a retinal detachment, it would be painless. Diagnosis requires a dilated eye exam with a qualified medical provider. In addition to the exam, a retina specialist may utilize state-of-the-art equipment, such as Optical Coherence Tomography (OCT) imaging, Ocular Ultrasound, and Fundus Photography to aid in diagnosis.
Treatment for a Retinal Detachment
There are a variety of treatments available for Retinal Detachments, including both surgical and non-surgical options. Our staff at Venice Retina will evaluate your specific situation and recommend a treatment plan to fits your needs!
Clinical Treatments:
Pneumatic Retinopexy – this option avoids the operating room and is instead an in-office procedure. In this scenario, the eye is numbed with topical drops, and a gas bubble is injected into the eye. The gas bubble will push the retina back into its original position. Days later, retinal laser is performed to tack the retina down in the area of the original tear. Over 3-4 weeks, the gas bubble will slowly decrease in size. While the gas bubble is present, you are not able to fly until the gas bubble dissipates.
This procedure is only performed for certain types of retinal detachments. Dr. Shane will advise if you are a good candidate for a Pneumatic Retinopexy!
Laser:
Some retinal detachments are small or chronic with a lower chance of immediate progression through the center of the vision. These detachments may be walled off by a line of retinal laser administered in the clinic. The advantage of this method is that it is non-invasive with low risk for complications. The laser does not ‘fix’ the retinal detachment per se but stops it from progressing towards the center of the vision. Most retinal detachments, however, require more invasive procedures to adequately protect the vision from imminent damage.
Surgical Treatment:
Vitrectomy: This is an outpatient surgical procedure where the vitreous jelly inside of your eye is removed, a laser is applied to the area of detached retina, and then either a gas or oil bubble is injected into the eye to read here the retina back to its original position at the back of the eye wall. If gas is utilized, there may be postoperative positioning requirements (for example, face down or upright only) to ensure that the gas bubble does its job in rendering the retina to its original position.
Scleral Buckle: This is an outpatient surgical procedure where a silicone band will be wrapped around the eyeball (think of placing a rubber band around a balloon!). It places an indentation on the eye wall, providing extra support to the retina and bringing the eye wall closer to the detached retina. The scleral buckle remains in place permanently around the eye following surgery. You are not able to see the scleral buckle nor are others able to as it is hidden behind the eye lid. A scleral buckle does cause a shift in your glass’s prescription towards near-sightedness. If you have a current glasses prescription, it will need to be updated following surgery.
Will I Regain My Vision If I Have A Retinal Detachment?
Delaying care or treatment can cause irreversible vision loss. If addressed quickly, the visual outcome tends to be better. The longer it goes untreated, the higher the risk of permanent vision loss. Many patients who seek care immediately regain back much of their previous vision!
I Think I Have A Retinal Detachment – What Should I Do?
As mentioned earlier, a retinal detachment is an urgent condition and is vision threatening. Dr. Anita Shane at Venice Retina specializes in diagnosis, treatment, surgical repair, and management of retinal detachments – if you have any signs or symptoms of a retinal detachment, please contact us today to seek care within 24 hours.
