What Is Diabetic Retinopathy?
You may have a close friend or family member who has diabetes, and some of the negative consequences this can have on health. While diabetes can have a variety of effects in the body, a particularly dangerous risk of elevated blood sugar is irreversible vision loss. It is important for patients to be well-informed about their diabetes diagnosis, including all potential ocular side effects. Prompt eye examination and evaluation can prevent damage to your vision.
What is Diabetes?
According to the American Diabetes Association (ADA), about 35 million Americans (10.5% of the population) have diabetes. Diabetes is characterized by high levels of blood sugar (also referred to as blood glucose). The circulating blood glucose in your body comes primarily from the foods you eat. Once we ingest a certain food, a cascade of hormones is activated inside of our body so that our blood sugar levels are at a constant state – not too high, and not too low. If, for example, we are eating a meal high in sugar like ice cream, our blood glucose level will rise, activating the release of insulin, a hormone created in the pancreas that works to decrease blood sugar levels. Insulin causes the cells in your body to absorb the blood sugar from the circulating blood and use it as fuel to power other energy-consuming processes, like exercising, metabolism, and vision. In diabetes, the underlying problem is that insulin does not work properly – it is unable to maintain a stable amount or level of blood glucose in the body. The sugar becomes trapped in our bloodstream and is unable to enter our cells. Thus, our cells are not able to absorb the sugar from the meal we eat, meaning that there is no fuel to provide energy for daily functions, causing a vicious cycle of prolonged elevated blood glucose levels.
There Are 2 Types of Diabetes
Type 1 (IDDM – Insulin Dependent Diabetes Mellitus)
Type 1 diabetes occurs when your body does not create insulin. Thus, your body is unable to manage its own blood sugar levels naturally, and requires daily insulin administration, typically in the form of a shot or a port. Patients who are type 1 diabetics are typically diagnosed during childhood.
Type 2 (NIDDM, Non-Insulin Dependent Diabetes Mellitus)
With type 2 diabetes, your body still produces insulin, but does not use it properly, resulting in an inability to regulate blood glucose levels. Type 2 diabetes is most commonly diagnosed during adulthood. The treatment for type 2 diabetes varies – some patients are required to utilize insulin injections, whereas others are primarily managed with medications and lifestyle changes.
Diabetes can cause a variety of health issues, including changes in your vision and other eye problems. In fact, diabetes is the leading cause of vision loss in people between the ages of 20 and 64.
How Does Diabetes Affect My Eyes?
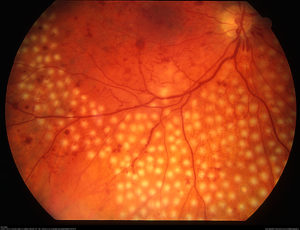
Diabetes can have many side effects that present in your eyes. One of the main underlying problems is that high levels of blood sugar damage the delicate blood vessels inside the retina. Our eyes are lined with fine, water-tight blood vessels that supply blood and oxygen to the retina, promoting vision. This constant enrichment of oxygen-rich blood is critical to the proper functioning of our eyes. While the blood vessels may be small in size, they are constantly working to keep up with the high levels of energy that the eye requires to produce vision.
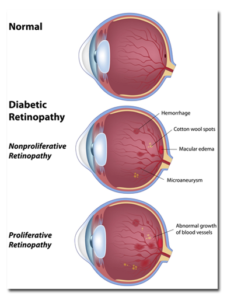
The prolonged elevated blood sugar causes the once water-tight blood vessels to become leaky, causing fluid to seep out into the retina. This back up of fluid inside the retina causes swelling and distortion directly in the center of your vision, a condition called diabetic macular edema (DME). Diabetic macular edema is the leading cause of vision loss in people with diabetes.
When your blood sugar is elevated for a prolonged period of time (such as months or even years), the retinal blood vessels become less and less effective at delivering an adequate oxygenated blood supply to your eyes. Thus, in this ‘oxygen-deprived state’, your body releases a chemical signal, called VEGF, or vascular endothelial growth factor, to stimulate new blood vessels to grow inside the eye. The growth of new blood vessels is termed neovascularization, and the presence of neovascularization represents the most advanced stage of diabetic eye disease – Proliferative Diabetic Retinopathy (PDR).

While the intention of growing new blood vessels inside the eye may appear to be beneficial, these are not normal blood vessels. They are considered faulty, bad blood vessels and can cause irreversible problems if not appropriately addressed. These blood vessels grow in an unpredictable way – they bleed into your eye and cause spontaneous hemorrhages, leading to sudden distortions in vision. They can also pull on your retina, causing a retinal detachment and severe vision loss.

I just was recently diagnosed with diabetes, but do not notice any change in my vision. Should I still see an Ophthalmologist?
According to the American Academy of Ophthalmology, it is recommended that adult diabetics receive a dilated eye examination every year. Many times, diabetic patients have underlying problems in their eyes that will be recognized during an eye exam, even though they may not necessarily notice a change in vision. The key to preventing diabetic vision loss is early treatment. A qualified eye doctor will be able to examine for any signs of blood vessel damage, growth of new blood vessels, or swelling in the retina. If treatment is delayed or too late in disease progression, your vision is at risk of being irreversibly lost, regardless of any treatment that is provided.
Signs And Symptoms of Diabetes in The Eye
The most common symptom with diabetic retinopathy is blurry or distorted vision. This can happen in one eye or both. This change in vision is typically painless and is sometimes associated with an acute onset of floaters. Floaters are small, mobile opacities in your vision. New floaters may represent a vitreous hemorrhage, or bleeding of the blood vessels into the jelly that fills your eye. Sometimes, diabetic patients can experience an increase in intraocular pressure, which can incidentally cause headaches.
It is important to test your vision in each eye independently of the other. In other words, you should cover one eye and evaluate your vision in one eye at a time, as the stronger eye can compensate for the weaker one with both eyes open.
Potential Treatment Options for Diabetic Retinopathy
While there are a variety of treatment options available to treat diabetic retinopathy or other diabetic related eye diseases, it is important to remember that the most powerful tool lies in lifestyle modifications, most importantly in maintaining good blood sugar control. The better your blood sugar and A1c values are, the less risk for vision loss. Other lifestyle modifications include controlling cardiovascular risk factors. These include stopping smoking, exercising frequently, and ensuring a healthy weight. It is also important to follow-up regularly with your primary care physician to prevent and treat high blood pressure (Hypertension) and high cholesterol (Hyperlipidemia) as these can also increase the chance of causing vision problems.
There are three main treatments employed for treating Diabetic Retinopathy:
Option #1 : Laser
This is an in-office procedure in which your retina specialist will numb the eye and apply a laser treatment to the retina in the back of the eye. This laser is applied specifically to the bad blood vessels in your eye that are causing leakage of fluid into the retina. The laser essentially seals off the vessel from leaking with the goal of reducing the swelling in the macula (DME) and preventing any further vision loss. Laser may also be used to prevent new blood vessels from growing into the eye.
Option #2: Eye Injections
This is also an in-office procedure where your retina specialist will apply an injection of medicine into the eye. In diabetic eye diseases, your body releases a chemical called VEGF (vascular endothelial growth factor) to stimulate bad blood vessels to grow inside the eye. The eye injection involves medications called anti-VEGF, that works to decrease swelling in the eye and stop the growth of faulty new blood vessels. The most common anti-VEGF medications are Avastin, Eylea, and Lucentis.
It is important to note that if you receive eye injections for a diabetic eye disease, you will have repeat injections several times per year. It is absolutely possible that by maintaining proper injection intervals recommended by your retina specialist, you can stop injections altogether once your disease progression has returned to its baseline.
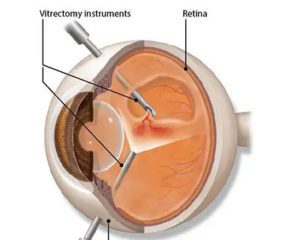
Option #3: Surgery
There are certain times in the more advanced cases of diabetic retinopathy that your retina specialist may recommend surgery. In this scenario, the vitreous jelly that fills the middle of the eye is removed and the retina is treated with laser to prevent future bleeding and retinal detachment., The surgery is a painless outpatient procedure called a Vitrectomy.
What Should I Do Next?
Dr. Anita Shane has years of experience in treating diabetic retinopathy and administering appropriate treatment plans for her patients. If you have diabetes, especially if you experience vision changes, please consider contacting our office for a dilated eye examination! There are many options available, and Dr. Shane will be happy to work with you to prevent any vision loss due to diabetic eye disease.
