Macula Edema Information
Located in the center most region of the retina is the macula. Measuring at 5mm in diameter, the macula is responsible for your central pinpoint vision. Within the macula is a high concentration of cells known as cone photoreceptors cells. These cells are responsible for our color vision and give us the ability to see fine details. These cells send signals directly to the brain to produce the outside world that you see. Maintaining a healthy macula is crucial for everyday activities such as driving, watching TV, using the computer, and recognizing faces. Damage to the macula, if left untreated, can lead to vision loss.
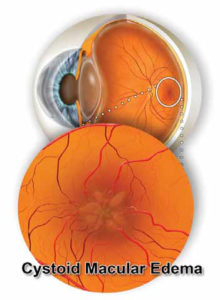
What Is Macular Edema?
Macular edema, also known as swelling in the macula, is a condition in which pockets of fluid begin to leak into the macula. Leakage of fluid into the macula occurs from damaged blood vessels that are within and around the layers of the retina. When there is an abnormal leakage of damaged blood vessels nearby, an accumulation of fluid causes the macula to swell and thicken leading to distorted vision.
The most common conditions that produce macular edema include diabetic retinopathy, age-related macular degeneration, and retinal vein occlusion. Additional, but less common factors, that may lead to macular edema include uveitis – an inflammatory eye disease – eye surgery, such as cataract extraction, and hypertension. Swelling caused by these three factors is known as cystoid macular edema (CME).
CME is a common side effect to any eye surgery, in particular cataract extraction. Inflammation that occurs in the surgical eye post-operation can cause the vessels within the macula to leak. This leakage leads to swelling in the macula which may result in an unexpected decrease of central vision. However, over time CME developed after cataract surgery may resolve with or without intervention from a retina specialist.
What Are the Symptoms of Macular Edema?
Macular edema creates a painless blur or waviness of central vision. Often, patients note a washed-out appearance of color, and they may experience more difficulty reading. Macular edema does not cause irritation, double vision, or pain to the eye. If only one eye is affected by macular edema, these symptoms may go unnoticed until the condition has advanced.
I Have Symptoms of Macular Edema, Now What?
If you are experiencing any of the mentioned symptoms it is important to be seen by an ophthalmologist so they can fully examine your eye to determine the underlying causes to your symptoms. During your visit with an ophthalmologist, a series of diagnostic tests will be performed to look for any abnormalities. The following tests may be done to determine the location and extent of the condition:
Visual Acuity Test: This test is a common method used to identify vision loss related to macular edema. Using a standardized eye chart with rows that decrease in size, the patient will be asked to cover one at eye a time and read the eye chart presented in front of them. This test allows the ophthalmologist to determine if there has been a decrease in vision.
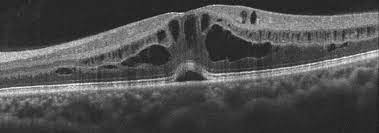
Optical Coherence Tomography:
An OCT machine is another diagnostic test that takes a closer look at the retina. This machine is one of the best ways to diagnose and identify macular edema. OCT is a non-invasive scan that uses light to scan the retina providing a clear and detailed image of its thickness. An OCT is also useful to monitor the progression of macular edema once treatment has begun.
Dilated Eye Exam: During this exam, drops are placed into the eye to dilate (widen) the pupils. This exam allows the ophthalmologist to thoroughly examine the retina and look for any abnormalities. Additionally, during this exam, the ophthalmologist will be able to detect the presence of abnormal or leaky blood vessels within the retina.
Fluorescein Angiogram:

With a combination of these diagnostic tools, your ophthalmologist will be able to discuss the appropriate treatment options for you.
What Treatment Options are Available for Macular Edema?
Accurately determining the underlying cause for macular edema is crucial for generating the appropriate treatment options. Dependent on the cause of your macular edema, treatment options may include:
Injections: Patients who develop macular edema in conjunction with macular degeneration and/or diabetic retinopathy will benefit from intraocular injections. These medications are known as anti-VEGF drugs that aid in reducing the abnormal growth of blood vessels into the retina. Injection of anti-VEGF drugs also decrease leakage preventing swelling in the macula. The most common anti -VEGF medications include, Eylea, Avastin and Lucentis. Note, it may be necessary for a series of anti-VEGF injections to take place to reduce swelling within the retina. Following the recommended injection interval given to you by your ophthalmologist is crucial in managing this condition. Once the swelling in the eye has reduced, it may be determined that injections can be discontinued.
Laser Treatment:
Development of macular edema in those with diabetic retinopathy may benefit from laser therapy. During this in office procedure, the ophthalmologist will first numb the effected eye then apply tiny laser spots to areas of leakage on the retina. During the procedure the ophthalmologist will avoid the center of the macula to prevent damage to the central vision. The goal of this procedure is to seal off leaking blood vessels to preserve and stabilize the patient’s vision.
Eye Drops: If cystoid macular edema presents itself after eye surgery, an ophthalmologist may prescribe non-steroidal anti-inflammatory eye drops over the next few months to reduce swelling in the eye. Regular office visits with OCT imaging will allow the ophthalmologist to determine the correct drop regimen for you.
Steroid Treatment: If it is determined that uveitis – an inflammatory eye disease – is the underlying cause for edema, steroid drops will be given to the patient initially until lab results can be obtained. Once a specific infection or autoimmune disorder is discovered, the patient may be treated with steroid medication or antibiotics. This treatment may be given in the form of eye drops, pills, or injections. The ophthalmologist may also consider a consultation with a rheumatologist for further management of medications.
What Are the Outcomes After Treatment?
Successful treatment of macular edema is possible. Given the cause of edema, with appropriate treatments and time, many patients rid themselves of swelling. Although full recovery of macular edema may not be possible for some, continued treatment will allow for stabilized vision.
Contact Us!
Dr. Anita Shane has years of experience in diagnosing, treating, and managing macular edema.
If you are experiencing any signs or symptoms related to macular edema, consider having a dilated eye exam. This exam may also consist of specialized testing and photographs to determine appropriate treatment. Macular edema has many effective treatment options, so contact Venice Retina today!
