Membrane Peel: An Effective Surgical Intervention
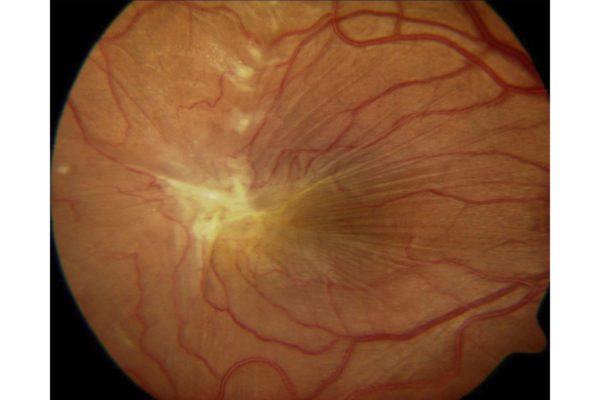
The retina is the light-sensitive tissue located in the back of the eye that transmits signals to your brain to produce the image you see. Within the retina are specialized cells known as photoreceptors. The most densely populated area of photoreceptors within the retina is known as the macula. When the clear gel-like fluid of the eye, known as the vitreous, naturally separates from the back of the eye, a very thin layer of scar tissue commonly forms on the surface of the retina. This tissue is known as an epiretinal membrane, more commonly referred to as a macular pucker . This pucker can cause the retina to wrinkle, ultimately distorting vision. In other cases, this scar-like tissue can pull the retina apart, causing a macular hole . Patients experiencing symptoms from a macular pucker or macular hole may benefit from surgical intervention involving a retinal membrane peel.
What is a Retinal Membrane Peel?
Since there are no drops, medications, or supplements to alleviate the symptoms of a macular pucker or macular hole, surgical intervention is the only available treatment. The surgery that takes place to remove a retinal membrane is known as a vitrectomy with a membrane peel. This common procedure is performed in an outpatient surgery center and takes approximately 45 minutes to complete. Patients are given local numbing around the eye to prevent the patient from feeling any pain or discomfort during the procedure.
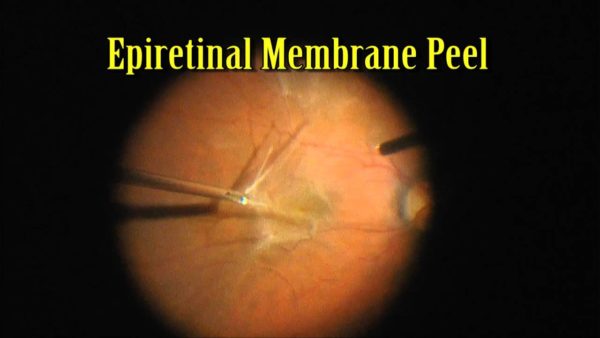
During this procedure, three tiny incisions are made through the white part of the eye – the sclera. One of the incisions will hold the surgeon’s light source and another will be the vitrector instrument. The vitrector cuts and sucks out the vitreous located in the center of the eye. This will allow the retinal surgeon to gain full access to the back of the eye. Forceps (microscopic tweezers) are then used to gently tug the retinal membrane off the surface of the retina. This relieves any tension placed on the retina allowing it to begin to relax. A saline solution is placed into the eye and within 24 hours your eye will naturally replace this solution with its own fluid.
In the case of patients who have a macular hole, similar surgical steps are performed. However, the vitreous space is replaced with gas through an intravitreal gas injection. This gas bubble will push the edges of the retina in place, allowing the macula to form back to its original position. Patients who are injected with a gas bubble will be required to remain in a face-down position for several days after surgery. This positioning, although often difficult, allows the gas bubble to press against the back of the eye, assisting the retinal tissue to return to its natural position. The gas bubble will remain in the eye for 2-8 weeks. During this time, your vision may be cloudy. As the gas bubble naturally reabsorbs on its own, the bubble will decrease in size allowing your vision to gradually return. Once the gas bubble is gone, typically the macular hole has closed, and your vision has returned to normal.
Do I Need a Retinal Membrane Peel?
In most cases, patients who have a macular pucker have mild symptoms. Epiretinal membranes are frequently found on imaging during routine eye exams. Those with mild epiretinal membranes experience near-normal vision with little distortion. As time passes, the epiretinal membrane or “wrinkle” may gradually tighten, producing worsening symptoms. Straight lines or words may appear as waves or blurred. It may become difficult to read fine print. Additionally, some patients may experience double vision. It is important to note that these symptoms are painless and will not lead to total blindness. Retinal membrane peels are an elective procedure and should be done in patients who are experiencing daily difficulties in their vision.
Unlike macular pucker, patients who have a macular hole should undergo surgical intervention in most cases. The longer a macular hole is left untreated, the worse your vision becomes. I also becomes less likely that the hole will close with delayed surgical intervention.

What is the Expected Outcome?
Thanks to advancements in surgical techniques and instrumentation, incision made during surgery are typically self-healing and require no sutures. This allows for faster healing time with minimal pain after surgery. On the day of surgery, patients go home with a patch over the surgical eye. The following day during the first post-operative appointment, the patch is removed. Some may notice the white part of the eye appears red, which will clear up over the first few weeks. Post-operative drops are frequently prescribed to reduce the risk of infection or inflammation in the first month. During the first few weeks of healing the retina will begin to relax back to its original state. Gradually over several months, vision continues to improve. Visual improvement from a retinal membrane peel varies based on multiple factors. These include:
- Severity of the macular pucker
- The length of time the pucker has been present
- Other concomitant eye conditions
The success rate for retinal membrane peels for epiretinal membranes and macular holes is high. Most patients experience a significant improvement in the vision and a decrease in visual distortion. Improvement in the vision after a retinal membrane peel continues for several months or even up to one year.
What Is the Risk of Macular Pucker Surgery?
As with any surgical procedure there are risks that must be considered before proceeding with a retinal membrane peel. The most common risk factors of a retinal membrane peel include:
- Post-operative infections or endophthalmitis – Any time surgery is performed in the eye, there is a risk for developing an infection. However, retinal surgeons take extra precaution during the procedure to limit the possibility of developing an infection. Sterile technique is utilized during the procedure, antibiotics are placed into the eye after surgery, and patients are placed on antibiotic drops during recovery. Despite these precautions there is still a small chance infection can occur. If an infection happens, it can be treated immediately to lessen the chance of permanent vision loss.
- Bleeding – Although blood loss during retina surgery is minimal, bleeding is another complication that may arise during the time of the procedure. It is important to discuss all medications prior to surgery. A retinal surgeon may recommend to discontinue the use of any blood thinners to reduce the chance of bleeding during surgery.
- Retinal tear or detachment – Vitrectomy surgery involves a 1% risk for retinal tear or retinal detachment. As the gel-like fluid is being removed from the eye, there is a chance that it takes a piece of the retina with it. At the end of every vitrectomy procedure, a 360-degree examination is performed to ensure there are no tears or detachments. If this occurs, laser treatment at the time of surgery will be performed to repair the retina. Retinal tears or detachments that occur after membrane peel surgery is complete require a return trip to the operating room. As with any retinal detachment, there is a risk for permanent vision loss.
- Progression of a cataract – Patients who have not yet undergone cataract extraction have a higher risk of developing a cataract. A vitrectomy procedure can accelerate the formation of a cataract. However, patients who have already had cataract surgery should not be concerned by this.
Dr. Anita Shane has successfully performed thousands of successful vitrectomies and retinal membrane peels for macular puckers and macular holes. If you are experiencing any symptoms related to a macular pucker or macular hole, schedule a consultation today!
