What is a Macular Hole?
To better understand what a macular hole is and the symptoms that this condition causes, we first need a quick lesson in eye anatomy. The retina is the light sensitive nerve tissue lining the back of our eyes that transmits signals to the brain to promote vision. The retina is made up of specialized cells called photoreceptors. The photoreceptors are located throughout the retinal tissue, but are most densely populated in the very center-most portion of the retina – the macula.
Just like the elbow is an anatomical location on your arm, the macula is an anatomical location in the retina. While the macula may only be 5 millimeters in length, it processes all of our sharp, detailed, central vision that we use for executing critical daily tasks such as reading, driving, and navigating through spaces. Your macula is responsible for processing the center of your sight. For example, if you are glancing at a picture of a loved one standing in front of the ocean, your macula will process the details of their face, such as their mouth, nose and hair color, whereas other parts of your retina will interpret the peripheral aspects of the photograph, such as the surrounding scenery and young children playing in the sand to the left and the right
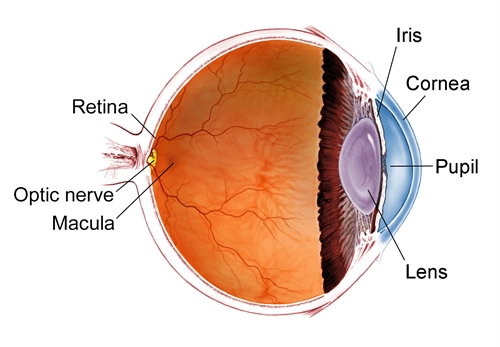
In front of the retina is the clear, gel-like fluid that fills the eye called the vitreous humor. The vitreous is attached to the retina through millions of microscopic fibers. As you grow older, the vitreous becomes increasingly liquified and naturally shrinks and pulls away from the surface of the retina, causing a tugging force on the sensitive macular tissue. A macular hole most commonly occurs when the vitreous is especially adherent to the macula, generating a stretching force on the retina that causes the macular tissue to pull apart, forming a hole.
What Causes a Macular Hole?
It is important to mention that there is almost nothing a patient can do to prevent a macular hole. Holes cannot be avoided by eating a well-balanced diet, nor can they be avoided by optimizing your overall health (though both are still important to do!). As mentioned previously, the most common cause of a macular hole occurs spontaneously when the vitreous jelly naturally separates from the retina. On the other hand, there are still some factors that place you at a higher risk of developing a macular hole:
- History of trauma or blunt injury to the eye. Most head or eye injuries will not cause a macular hole, however.
- History of a macular hole in your other eye. Patients that develop a macular hole in one eye are at an increased likelihood of developing it in the opposite eye.
- Underlying macular pucker (AKA epiretinal membrane). If you have been diagnosed with a macular pucker, this can sometimes exacerbate the tugging force that occurs when the vitreous separates from the retina.
Signs and Symptoms of a Macular Hole?
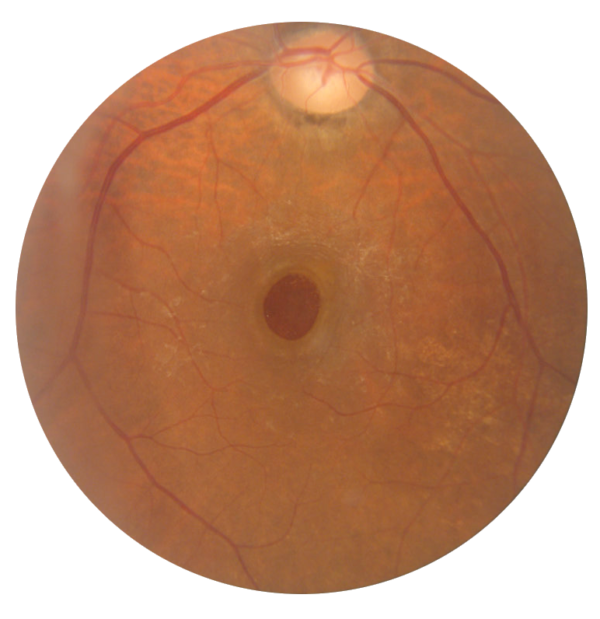
The most common symptom of a macular hole is painless loss of central vision in one eye. Since the macula is the center of your vision, a hole in this area will cause an associated central blind spot. Since the retina does not have any pain receptors, it will not be associated with any pain or discomfort.
If a macular hole develops in your less dominant eye, it may go unrecognized as our eyes are known to compensate for each other. To test this, cover one eye at a time and evaluate each eye independently to check for any central distortion or loss of vision.
Some patients with a macular hole may not notice a complete blind spot, but instead heavy, central distortion. For example, you may see lines as wavy or blurry, and have difficulty with reading, amongst other things.
Treatment Options for a Macular Hole
If you are experiencing a blind spot in your vision or suspect you may have a macular hole, it is important to seek prompt evaluation and treatment with an ophthalmologist specialized in retinal surgery. The longer that a macular hole goes untreated, the less likely it is to close with any type of intervention. There are, however, multiple avenues to treating a macular hole and restoring the your central vision. Your retina specialist will discuss these options with you and recommend a plan that fits your specific needs.

Option #1: Surgery
This option is a 45-minute, outpatient surgery that occurs under local anesthesia. During surgery, your physician will perform a vitrectomy, which involves removing the vitreous humor that fills the eye. Following this, a microscopic membrane will be peeled off your retina and a gas bubble will be injected into the inside of the eye, replacing the space that was once filled with vitreous jelly. The gas bubble aids in closing the hole and resealing the macula back to its original position.
Macular hole patients will go home the same-day, but since there is a gas bubble inside of the eye, patients are frequently required to spend a few days in face-down positioning. When we mention face-down positioning, we encourage looking towards to floor as much as possible. We recognize that this can be difficult, so it is something we discuss with you during consultation. Since the macula is in the back of the eye, when you are face-down, the gas bubble is pressing directly against the macula (at the back of the eye), resealing the hole and returning the retinal tissue to its intended position. While your hole may still close without face-down positioning, the risk for experiencing a persistent macular hole increases.
The gas bubble will be present in your eye for anywhere from 2-8 weeks and during this time your vision will be limited. As the gas bubble decreases in size during this time, your vision will gradually return. The macular hole is typically found to be completely closed and your vision returned to normal.
A side effect of this surgery is that it accelerates the formation of a cataract in the months after your procedure. Thus, once your macular hole is completely repaired, your vision may start to blur months later, in which case you may seek out cataract surgery. Additionally, when a gas bubble is present, you are unable to travel by plane or perform other activities where a change in altitude occurs (scuba diving, hiking a mountain, etc.).
Option #2: Pneumatic Vitreolysis
This option is an in-office, less-invasive procedure to treat a macular hole. While surgery is the most successful treatment to repair a macular hole, there are some instances when your retina specialist may recommend a pneumatic vitreolysis. During this procedure, a gas bubble will be injected into your eye. This gas will push against the vitreous humor and relieve the vitreous traction on the macula which is causing the macular hole. This release is sometimes enough to allow the hole to close, thus preventing the need for vitrectomy surgery.
Option #3: Topical Therapy
In a very few select cases, a macular hole can be small enough to close with eye drops. This is the least invasive option. However, drops are effective in only a small percentage of cases.
Will my health insurance cover this surgery?
Dr. Shane is in network with most major insurances, so surgery is typically covered subject to your copayments and deductibles.
I don’t know if I can do face-down positioning after surgery – what should I do?
The positioning requirements after a surgery requiring a gas injection in the eye are strenuous. Even if you don’t position at all, there is still a good chance that your macular hole will close. However, the chances of successful surgery are increased with face-down positioning. There are some options to make the positioning requirements easier, such as in-home equipment designed to make a face-down position more comfortable and convenient. This equipment is often covered by insurance, too! Dr. Shane will discuss all of the risks, benefits, and alternatives to treatment with you during your consultation and answer any questions you may have!
What Should I Do Next?
If you are experiencing any distortion or a new blind spot in your central vision (in one or both eyes), it is important to schedule a prompt dilated eye examination with a qualified ophthalmologist. Your physician will dilate your eyes to be able to properly evaluate your retina (where a macular hole occurs), check your intraocular eye pressure, and obtain specialized imaging of your eyes. Dr. Shane specializes in macular hole repairs, having performed countless operations to repair them and restore vision to her patients. Please do not delay your evaluation – contact our office today!
