What is a Retinal Vein Occlusion?
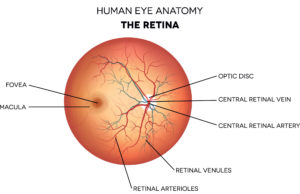
Before understanding what a retinal vein occlusion is, let’s first discuss how blood flows throughout our bodies. Arteries are blood vessels that carry oxygenated blood away from the heart to distant parts of our body, such as the arms and legs. Veins, on the other hand, are blood vessels that return deoxygenated blood from these distant parts, such as our fingers and toes, back to the heart. Arteries and veins work in conjunction to circulate blood to all of our necessary internal organs, tissues, and accessory structures. They are located all over our body – even in our eyes! The retina, a light-sensitive tissue lining the back of our eyes, works to transmit light to our brain, creating vision. Vision itself is a very energy-consuming process, requiring a constant enrichment of blood and nutrients to sustain itself. It is critical that our eye is constantly receiving appropriate blood flow at all times – our vision depends on it!
A retinal vein occlusion is the blockage of blood flow in one of the veins of your retina. Recall that veins return the blood back to the heart. When a retinal vein is blocked, or “occluded”, blood is unable to exit the eye on its way back to the heart, and instead begins to back up inside the eye. The blood begins to pool and leak into the retina, causing distortions in your vision.
There are two main types of retinal vein occlusions: a central retinal vein occlusion (CRVO) and a branched retinal vein occlusion (BRVO).
What is the Difference Between a CRVO and a BRVO?
Anatomically speaking, there are two main categories of veins inside the eye. The central retinal vein is the largest vein, located right in the center of your vision. When the central retinal vein branches off into smaller blood vessels, they are referred to as branched retinal veins. For illustrative purposes, imagine a large, flowing river with smaller streams or tributaries branching off of it as it progresses downstream. The main river itself represents the central retinal vein, whereas the smaller streams that branch off of it can be thought of as the branched retinal veins. The location of your occlusion correlates to the diagnosis you receive. In other words, if your occlusion is located in the central retinal vein, you are diagnosed with a CRVO.
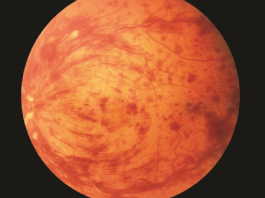
A central retinal vein occlusion (CRVO) is when the single, large vein that drains blood from the retina becomes blocked. The central retinal vein exits the eye through the optic nerve, and the blockage typically occurs at this site. Since the central retinal vein is the only location for blood to exit the eye itself, a blockage has serious side effects that patients usually notice immediately. It can cause hemorrhages, swelling in the central retina, and a decrease in vision, typically affecting the entire visual field of one eye. Continuing with the previous analogy, you can compare a CRVO to a large boulder falling right into the main river, causing a backup of water upstream – the boulder creates an impenetrable boundary so that the water is unable to pass through.
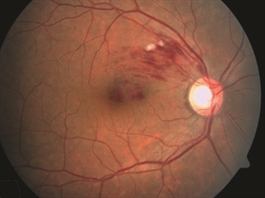
A branched retinal vein occlusion (BRVO) occurs when a tributary of the central retinal vein is blocked. A BRVO typically occurs at a point inside of the retina where a branch of the retinal artery and retinal vein overlap. At this junction, the stiff-walled artery can press down on the soft-walled vein, causing the vein to collapse. This obstructs the blood flow, resulting in hemorrhages and swelling of the retina. Unlike CRVO’s, BRVO’s typically do not affect the entire visual field. Going back to the river analogy, a BRVO would be when the boulder falls in one of the peripheral streams, impeding water from flowing.
Symptoms Associated With a Retinal Vein Occlusion
If you experience a sudden, painless decrease in vision, you may have a retinal vein occlusion. Typically RVO’s are localized to one eye. A CRVO will cause blurred vision throughout the entire field of vision, meaning that both your central vision and peripheral vision will be affected. A BRVO, on the other hand, typically only affects a subset of your vision – usually the upper or lower parts of your peripheral vision, though the central vision can still be affected.
In some instances, patients may not notice a significant distortion in their vision as our eyes often work together and one eye may compensate for the decrease in vision of the other eye. To evaluate each eye independently, cover one eye with your hand and monitor your vision then do the same for the opposite eye. If you notice one eye is suddenly increasingly blurry, it is important to be evaluated quickly.
How is a Retinal Vein Occlusion Diagnosed?
If you have a sudden decrease in vision, especially in one eye, it is important to seek a prompt dilated eye exam with an ophthalmologist, specifically a retina specialist. The sooner that your RVO is evaluated and diagnosed, the better prognosis of your visual outcome.
At your ophthalmology appointment, your eyes will be dilated and your vision will be assessed. Your ophthalmologist will also obtain specialized imaging of your retina, such as an OCT (Optical Coherence Tomography) or fundus photography to evaluate if there is any blood, swelling, or hemorrhage in the eye.
Your retina specialist may also send you for an appropriate laboratory work-up if applicable as retinal vein occlusions can sometimes be related to other systemic diseases, such as autoimmune conditions.
What Causes a Retinal Vein Occlusion?
Many of the same risk factors that place patients at an increased risk of a heart attack or stroke also put you at an increased risk of a retinal vein occlusion. These include:
- Age: Patients older than 50 have a higher risk of developing a retinal vein occlusion.
- High blood pressure (Hypertension): High blood pressure can cause the arteries in our body to become more stiff and inflexible, causing a higher risk of a blood clot or “occlusion” to form. It is important to monitor your blood pressure with your primary care physician or cardiologist to mitigate these risks.
- Heart disease or Diabetes
- Obesity
- High cholesterol (Hyperlipidemia)
- Smoking
- Poor diet and/or lack of exercise
If you are diagnosed with a retinal vein occlusion and are younger than 50 years of age, it is important to be evaluated for other conditions such as autoimmune diseases, clotting disorders, or other blood or hematological disorders including cancer.
How Do You Treat a Retinal Vein Occlusion?
There are a variety of treatment options available to treat a retinal vein occlusion – your retina specialist will evaluate you and recommend a plan that works for your unique needs!
Treatment Option #1
Intravitreal Injections. This is a shot of medication into the eye aimed at decreasing the swelling in your retina and resolving any hemorrhages that are present. Injections may have to be repeated over the course of 4-12 weeks, with the intention of extending to months or even years.
Treatment Option #2
Laser Treatment. This option is usually initiated in the rare event that injections are not effective. This is additionally warranted in the event of a retinal vein occlusion that causes the growth of new blood vessels in the eye. Laser is applied to the retina at the back of the eye. This prevents the blood vessels from growing and leaking into the retina causing swelling or hemorrhage.
Treatment Option #3
Observation. In some instances of retinal vein occlusions that occur outside of the center of your vision and do not cause any swelling or hemorrhage, your retina specialist can safely monitor you without treatment.
Prognosis
Timely diagnosis and treatment is critical in the prognosis of a retinal vein occlusion. Many patients experience excellent vision when appropriate treatment is initiated promptly, often recovering the vision that was suddenly lost. Delaying treatment is the most common cause of vision loss or poor visual prognosis. Sometimes, a retinal vein occlusion can be unresponsive to any form of treatment due to the lack of blood flow, causing irreversible vision loss.
Contact Us Today!
Dr. Anita Shane has years of training and experience in assessing, diagnosing, and treating retinal vein occlusions. She will recommend an appropriate treatment plan to fit your needs! If you have any signs or symptoms of a retinal vein occlusion, or even have underlying conditions that place you at an increased risk of developing a RVO, contact Dr. Shane at Venice Retina today for expert eye care!
